Addressing Fallen Arches
Overview
Because young children are unlikely to suspect or identify flat feet on their own, it is a good idea for parents or other adult caregivers to check on this themselves. Besides visual inspection, parents should notice whether a child begins to walk oddly or clumsily, for example on the outer edges of the feet, or to limp, during long walks, and to ask the child whether he or she feels foot pain or fatigue during such walks. Children who complain about calf muscle pains or any other pains around the foot area, may be developing or have flat feet. Pain or discomfort may also develop in the knee joints. A recent randomized controlled trial found no evidence for the efficacy of treatment of flat feet in children either for expensive prescribed orthoses (shoe inserts) or less expensive over-the-counter orthoses.
Causes
When flat feet develop at a later age, they are known as fallen arches. The arches may fall because the muscles supporting them are no longer able to do so. In addition the spring ligament within the foot may have lost some of its tension allowing the arch of the foot to flatten. Other conditions causing fallen arches include sudden weight gain, a nervous system injury, or a loss of sensation caused by a disease such as diabetes. Most people with fallen arches are flat on both feet.
Symptoms
People will have a very heavily dropped arch and it won?t affect them at all and people will have it slightly dropped and it could cause fierce problems. It could cause things like plantar fasciitis, it could cause heel spurs, desperate ball-of-the-foot pressure, or pressure on the big toe known as the hallux which causes discomfort in the foot. It will create problems upwards to the knees, hips and the back once you?re out of line.
Diagnosis
People who have flat feet without signs or symptoms that bother them do not generally have to see a doctor or podiatrist about them. However, if any of the following occur, you should see your GP or a podiatrist. The fallen arches (flat feet) have developed recently. You experience pain in your feet, ankles or lower limbs. Your unpleasant symptoms do not improve with supportive, well-fitted shoes. Either or both feet are becoming flatter. Your feet feel rigid (stiff). Your feet feel heavy and unwieldy. Most qualified health care professionals can diagnose flat feet just by watching the patient stand, walk and examining his/her feet. A doctor will also look at the patient's medical history. The feet will be observed from the front and back. The patient may be asked to stand on tip-toe while the doctor examines the shape and functioning of each foot. In some cases the physician may order an X-ray, CT (computed tomography) scan, or MRI (magnetic resonance imaging) scan.
What is PES Planovalgus deformity?
Non Surgical Treatment
The typical treatment for pain from fallen arches is an arch insert. While many people experience dramatic pain relief from this, others continue to suffer from chronic achy feet despite the arch support. The problem with this approach is that it does not do anything to strengthen the weak ligaments that may be at the root of the problem and, thus, does not alleviate the chronic pain that people with this condition experience. Another standard practice of modern medicine is to use steroids or to prescribe anti-inflammatory medications. However, in the long run, these treatments do more damage than good. Cortisone shots and anti-inflammatory drugs have been shown to produce short-term pain benefit, but both result in long-term loss of function and even more chronic pain by actually inhibiting the healing process of soft tissues and accelerating cartilage degeneration. Plus, long-term use of these drugs can lead to other sources of chronic pain, allergies and leaky gut syndrome.
Surgical Treatment

Rarely does the physician use surgery to correct a foot that is congenitally flat, which typically does not cause pain. If the patient has a fallen arch that is painful, though, the foot and ankle physicians at Midwest Orthopaedics at Rush may perform surgery to reconstruct the tendon and "lift up" the fallen arch. This requires a combination of tendon re-routing procedures, ligament repairs, and bone cutting or fusion procedures.
Prevention
Orthotic inserts, either prescribed or bought over the counter, can help keep the arches fixed into position, but always wear them as although they support, they don?t strengthen, which is why some experts reccomend avoiding them. Gait analysis at a run specialist can help to diagnose overpronation and flat feet. Most brands produce shoes that will give support and help to limit the negative effects of a poor gait on the rest of the body. Barefoot exercises, such as standing on a towel and making fists with the toes, can help to strengthen the arches. Start easy and build up the reps to avoid cramping. Short barefoot running sessions can help take pressure off the arches by using the natural elasticity of the foot?s tendons to take impact and build strength to help prevent flat feet. These should be done on grass for only a few minutes at a time.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.
Because young children are unlikely to suspect or identify flat feet on their own, it is a good idea for parents or other adult caregivers to check on this themselves. Besides visual inspection, parents should notice whether a child begins to walk oddly or clumsily, for example on the outer edges of the feet, or to limp, during long walks, and to ask the child whether he or she feels foot pain or fatigue during such walks. Children who complain about calf muscle pains or any other pains around the foot area, may be developing or have flat feet. Pain or discomfort may also develop in the knee joints. A recent randomized controlled trial found no evidence for the efficacy of treatment of flat feet in children either for expensive prescribed orthoses (shoe inserts) or less expensive over-the-counter orthoses.
Causes
When flat feet develop at a later age, they are known as fallen arches. The arches may fall because the muscles supporting them are no longer able to do so. In addition the spring ligament within the foot may have lost some of its tension allowing the arch of the foot to flatten. Other conditions causing fallen arches include sudden weight gain, a nervous system injury, or a loss of sensation caused by a disease such as diabetes. Most people with fallen arches are flat on both feet.
Symptoms
People will have a very heavily dropped arch and it won?t affect them at all and people will have it slightly dropped and it could cause fierce problems. It could cause things like plantar fasciitis, it could cause heel spurs, desperate ball-of-the-foot pressure, or pressure on the big toe known as the hallux which causes discomfort in the foot. It will create problems upwards to the knees, hips and the back once you?re out of line.
Diagnosis
People who have flat feet without signs or symptoms that bother them do not generally have to see a doctor or podiatrist about them. However, if any of the following occur, you should see your GP or a podiatrist. The fallen arches (flat feet) have developed recently. You experience pain in your feet, ankles or lower limbs. Your unpleasant symptoms do not improve with supportive, well-fitted shoes. Either or both feet are becoming flatter. Your feet feel rigid (stiff). Your feet feel heavy and unwieldy. Most qualified health care professionals can diagnose flat feet just by watching the patient stand, walk and examining his/her feet. A doctor will also look at the patient's medical history. The feet will be observed from the front and back. The patient may be asked to stand on tip-toe while the doctor examines the shape and functioning of each foot. In some cases the physician may order an X-ray, CT (computed tomography) scan, or MRI (magnetic resonance imaging) scan.
What is PES Planovalgus deformity?
Non Surgical Treatment
The typical treatment for pain from fallen arches is an arch insert. While many people experience dramatic pain relief from this, others continue to suffer from chronic achy feet despite the arch support. The problem with this approach is that it does not do anything to strengthen the weak ligaments that may be at the root of the problem and, thus, does not alleviate the chronic pain that people with this condition experience. Another standard practice of modern medicine is to use steroids or to prescribe anti-inflammatory medications. However, in the long run, these treatments do more damage than good. Cortisone shots and anti-inflammatory drugs have been shown to produce short-term pain benefit, but both result in long-term loss of function and even more chronic pain by actually inhibiting the healing process of soft tissues and accelerating cartilage degeneration. Plus, long-term use of these drugs can lead to other sources of chronic pain, allergies and leaky gut syndrome.
Surgical Treatment

Rarely does the physician use surgery to correct a foot that is congenitally flat, which typically does not cause pain. If the patient has a fallen arch that is painful, though, the foot and ankle physicians at Midwest Orthopaedics at Rush may perform surgery to reconstruct the tendon and "lift up" the fallen arch. This requires a combination of tendon re-routing procedures, ligament repairs, and bone cutting or fusion procedures.
Prevention
Orthotic inserts, either prescribed or bought over the counter, can help keep the arches fixed into position, but always wear them as although they support, they don?t strengthen, which is why some experts reccomend avoiding them. Gait analysis at a run specialist can help to diagnose overpronation and flat feet. Most brands produce shoes that will give support and help to limit the negative effects of a poor gait on the rest of the body. Barefoot exercises, such as standing on a towel and making fists with the toes, can help to strengthen the arches. Start easy and build up the reps to avoid cramping. Short barefoot running sessions can help take pressure off the arches by using the natural elasticity of the foot?s tendons to take impact and build strength to help prevent flat feet. These should be done on grass for only a few minutes at a time.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.
Activities To Correct Leg Length Discrepancy
Overview
While many people have slight differences in the length of one leg compared to the other, a significant difference between the two legs can cause problems. Leg length discrepancies can disturb the way a person walks, how his or her spine lines up and strain hip joints.
Causes
Some children are born with absence or underdeveloped bones in the lower limbs e.g., congenital hemimelia. Others have a condition called hemihypertrophy that causes one side of the body to grow faster than the other. Sometimes, increased blood flow to one limb (as in a hemangioma or blood vessel tumor) stimulates growth to the limb. In other cases, injury or infection involving the epiphyseal plate (growth plate) of the femur or tibia inhibits or stops altogether the growth of the bone. Fractures healing in an overlapped position, even if the epiphyseal plate is not involved, can also cause limb length discrepancy. Neuromuscular problems like polio can also cause profound discrepancies, but thankfully, uncommon. Lastly, Wilms? tumor of the kidney in a child can cause hypertrophy of the lower limb on the same side. It is therefore important in a young child with hemihypertrophy to have an abdominal ultrasound exam done to rule out Wilms? tumor. It is important to distinguish true leg length discrepancy from apparent leg length discrepancy. Apparent discrepancy is due to an instability of the hip, that allows the proximal femur to migrate proximally, or due to an adduction or abduction contracture of the hip that causes pelvic obliquity, so that one hip is higher than the other. When the patient stands, it gives the impression of leg length discrepancy, when the problem is actually in the hip.
Symptoms
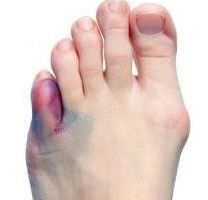
In addition to the distinctive walk of a person with leg length discrepancy, over time, other deformities may be noted, which help compensate for the condition. Toe walking on the short side to decrease the swaying during gait. The foot will supinate (high arch) on the shorter side. The foot will pronate (flattening of the arch) on the longer side. Excessive pronation leads to hypermobility and instability, resulting in metatarsus primus varus and associated unilateral juvenile hallux valgus (bunion) deformity.
Diagnosis
Infants, children or adolescents suspected of having a limb-length condition should receive an evaluation at the first sign of difficulty in using their arms or legs. In many cases, signs are subtle and only noticeable in certain situations, such as when buying clothing or playing sports. Proper initial assessments by qualified pediatric orthopedic providers can reduce the likelihood of long-term complications and increase the likelihood that less invasive management will be effective. In most cases, very mild limb length discrepancies require no formal treatment at all.
Non Surgical Treatment
In some circumstances, the physician will recommend a non-surgical form of treatment. Non-surgical treatments include orthotics and prosthetics. Orthotics are a special type of lift placed in or on a shoe that can be used in the treatment of leg length discrepancies between two and six centimeters. In pediatric patients who have large discrepancies and are not good candidates for other treatment forms, prosthetics can be helpful.

how do you get taller in a day?
Surgical Treatment
Many people undergo surgery for various reasons - arthritis, knee replacement, hip replacement, even back surgery. However, the underlying cause of leg length inequality still remains. So after expensive and painful surgery, follow by time-consuming and painful rehab, the true culprit still remains. Resuming normal activities only continues to place undue stress on the already overloaded side. Sadly so, years down the road more surgeries are recommended for other joints that now endure the excessive forces.
While many people have slight differences in the length of one leg compared to the other, a significant difference between the two legs can cause problems. Leg length discrepancies can disturb the way a person walks, how his or her spine lines up and strain hip joints.

Causes
Some children are born with absence or underdeveloped bones in the lower limbs e.g., congenital hemimelia. Others have a condition called hemihypertrophy that causes one side of the body to grow faster than the other. Sometimes, increased blood flow to one limb (as in a hemangioma or blood vessel tumor) stimulates growth to the limb. In other cases, injury or infection involving the epiphyseal plate (growth plate) of the femur or tibia inhibits or stops altogether the growth of the bone. Fractures healing in an overlapped position, even if the epiphyseal plate is not involved, can also cause limb length discrepancy. Neuromuscular problems like polio can also cause profound discrepancies, but thankfully, uncommon. Lastly, Wilms? tumor of the kidney in a child can cause hypertrophy of the lower limb on the same side. It is therefore important in a young child with hemihypertrophy to have an abdominal ultrasound exam done to rule out Wilms? tumor. It is important to distinguish true leg length discrepancy from apparent leg length discrepancy. Apparent discrepancy is due to an instability of the hip, that allows the proximal femur to migrate proximally, or due to an adduction or abduction contracture of the hip that causes pelvic obliquity, so that one hip is higher than the other. When the patient stands, it gives the impression of leg length discrepancy, when the problem is actually in the hip.
Symptoms
In addition to the distinctive walk of a person with leg length discrepancy, over time, other deformities may be noted, which help compensate for the condition. Toe walking on the short side to decrease the swaying during gait. The foot will supinate (high arch) on the shorter side. The foot will pronate (flattening of the arch) on the longer side. Excessive pronation leads to hypermobility and instability, resulting in metatarsus primus varus and associated unilateral juvenile hallux valgus (bunion) deformity.
Diagnosis
Infants, children or adolescents suspected of having a limb-length condition should receive an evaluation at the first sign of difficulty in using their arms or legs. In many cases, signs are subtle and only noticeable in certain situations, such as when buying clothing or playing sports. Proper initial assessments by qualified pediatric orthopedic providers can reduce the likelihood of long-term complications and increase the likelihood that less invasive management will be effective. In most cases, very mild limb length discrepancies require no formal treatment at all.
Non Surgical Treatment
In some circumstances, the physician will recommend a non-surgical form of treatment. Non-surgical treatments include orthotics and prosthetics. Orthotics are a special type of lift placed in or on a shoe that can be used in the treatment of leg length discrepancies between two and six centimeters. In pediatric patients who have large discrepancies and are not good candidates for other treatment forms, prosthetics can be helpful.

how do you get taller in a day?
Surgical Treatment
Many people undergo surgery for various reasons - arthritis, knee replacement, hip replacement, even back surgery. However, the underlying cause of leg length inequality still remains. So after expensive and painful surgery, follow by time-consuming and painful rehab, the true culprit still remains. Resuming normal activities only continues to place undue stress on the already overloaded side. Sadly so, years down the road more surgeries are recommended for other joints that now endure the excessive forces.
Addressing Mortons Neuroma
Overview
 A neuroma is a thickening of nerve tissue that may develop in various parts of the body. The most common neuroma in the foot is a Morton?s neuroma, which occurs between the third and fourth toes. It is sometimes referred to as an intermetatarsal neuroma. ?Intermetatarsal? describes its location in the ball of the foot between the metatarsal bones. Neuromas may also occur in other locations in the foot. MortonThe thickening, or enlargement, of the nerve that defines a neuroma is the result of compression and irritation of the nerve. This compression creates enlargement of the nerve, eventually leading to permanent nerve damage.
A neuroma is a thickening of nerve tissue that may develop in various parts of the body. The most common neuroma in the foot is a Morton?s neuroma, which occurs between the third and fourth toes. It is sometimes referred to as an intermetatarsal neuroma. ?Intermetatarsal? describes its location in the ball of the foot between the metatarsal bones. Neuromas may also occur in other locations in the foot. MortonThe thickening, or enlargement, of the nerve that defines a neuroma is the result of compression and irritation of the nerve. This compression creates enlargement of the nerve, eventually leading to permanent nerve damage.
Causes
Some say that this condition should not be called Morton's neuroma as, in fact, it is not actually a neuroma. A neuroma is a non-cancerous (benign) tumour that grows from the fibrous coverings of a nerve. There is no tumour formation in Morton's neuroma. The anatomy of the bones of the foot is also thought to contribute to the development of Morton's neuroma. For example, the space between the long bones (metatarsals) in the foot is narrower between the second and third, and between the third and fourth metatarsals. This means that the nerves that run between these metatarsals are more likely to be compressed and irritated. Wearing narrow shoes can make this compression worse.
Symptoms
Often, no outward signs (such as a lump or unusual swelling) appear from the condition. Neuroma pain is most often described as a burning discomfort in the forefoot. Aching or sudden shooting pain in the forefoot is also common. All running sports, especially distance running can leave an athlete vulnerable to Morton?s Neuroma, which may appear or flare up in the middle of a run or at the end. The sufferer often has the desire to remove his shoe and rub the afflicted foot. Should the Neuroma be of sufficient size, or if footwear is particularly tight or uncomfortable, the painful condition may be present during normal walking. Numbness in the foot may precede or accompany Neuroma pain.
Diagnosis
Your doctor will suspect that you have a Morton's neuroma based on the nature and location of your foot pain. He or she may ask questions about your shoes - what type of shoes you usually wear and whether these shoes have narrow toes or high heels. To rule out other causes of foot pain, your doctor may ask questions about your medical history, especially any history of arthritis, nerve and muscle problems or previous injury to your foot or leg.
Non Surgical Treatment
Treatment options vary with the severity of each neuroma, and identifying the neuroma early in its development is important to avoid surgical correction. For simple, undeveloped neuromas, a pair of thick-soled shoes with a wide toe box is often adequate treatment to relieve symptoms, allowing the condition to diminish on its own. For more severe conditions, however, additional treatment or surgery may be necessary to remove the tumor. The primary goal of most early treatment regimens is to relieve pressure on areas where a neuroma develops. Your podiatric physician will examine and likely X-ray the affected area and suggest a treatment plan that best suits your individual case. Padding and Taping. Special padding at the ball of the foot may change the abnormal foot function and relieve the symptoms caused by the neuroma. Medication. Anti-inflammatory drugs and cortisone injections can be prescribed to ease acute pain and inflammation caused by the neuroma. Orthotics. Custom shoe inserts made by your podiatrist may be useful in controlling foot function. Orthotics may reduce symptoms and prevent the worsening of the condition.
Surgical Treatment
About one person in four will not require any surgery for Morton's neuroma and their symptoms can be controlled with footwear modification and steroid/local anaesthetic injections. Of those who choose to have surgery, about three out of four will have good results with relief of their symptoms. Recurrent or persisting (chronic) symptoms can occur after surgery. Sometimes, decompression of the nerve may have been incomplete or the nerve may just remain 'irritable'. In those who have had cutting out (resection) of the nerve (neurectomy), a recurrent or 'stump' neuroma may develop in any nerve tissue that was left behind. This can sometimes be more painful than the original condition.
Prevention
Ensuring that shoes are well fitted, low-heeled and with a wide toe area may help to prevent Morton's neuroma.
 A neuroma is a thickening of nerve tissue that may develop in various parts of the body. The most common neuroma in the foot is a Morton?s neuroma, which occurs between the third and fourth toes. It is sometimes referred to as an intermetatarsal neuroma. ?Intermetatarsal? describes its location in the ball of the foot between the metatarsal bones. Neuromas may also occur in other locations in the foot. MortonThe thickening, or enlargement, of the nerve that defines a neuroma is the result of compression and irritation of the nerve. This compression creates enlargement of the nerve, eventually leading to permanent nerve damage.
A neuroma is a thickening of nerve tissue that may develop in various parts of the body. The most common neuroma in the foot is a Morton?s neuroma, which occurs between the third and fourth toes. It is sometimes referred to as an intermetatarsal neuroma. ?Intermetatarsal? describes its location in the ball of the foot between the metatarsal bones. Neuromas may also occur in other locations in the foot. MortonThe thickening, or enlargement, of the nerve that defines a neuroma is the result of compression and irritation of the nerve. This compression creates enlargement of the nerve, eventually leading to permanent nerve damage.Causes
Some say that this condition should not be called Morton's neuroma as, in fact, it is not actually a neuroma. A neuroma is a non-cancerous (benign) tumour that grows from the fibrous coverings of a nerve. There is no tumour formation in Morton's neuroma. The anatomy of the bones of the foot is also thought to contribute to the development of Morton's neuroma. For example, the space between the long bones (metatarsals) in the foot is narrower between the second and third, and between the third and fourth metatarsals. This means that the nerves that run between these metatarsals are more likely to be compressed and irritated. Wearing narrow shoes can make this compression worse.
Symptoms
Often, no outward signs (such as a lump or unusual swelling) appear from the condition. Neuroma pain is most often described as a burning discomfort in the forefoot. Aching or sudden shooting pain in the forefoot is also common. All running sports, especially distance running can leave an athlete vulnerable to Morton?s Neuroma, which may appear or flare up in the middle of a run or at the end. The sufferer often has the desire to remove his shoe and rub the afflicted foot. Should the Neuroma be of sufficient size, or if footwear is particularly tight or uncomfortable, the painful condition may be present during normal walking. Numbness in the foot may precede or accompany Neuroma pain.
Diagnosis
Your doctor will suspect that you have a Morton's neuroma based on the nature and location of your foot pain. He or she may ask questions about your shoes - what type of shoes you usually wear and whether these shoes have narrow toes or high heels. To rule out other causes of foot pain, your doctor may ask questions about your medical history, especially any history of arthritis, nerve and muscle problems or previous injury to your foot or leg.
Non Surgical Treatment
Treatment options vary with the severity of each neuroma, and identifying the neuroma early in its development is important to avoid surgical correction. For simple, undeveloped neuromas, a pair of thick-soled shoes with a wide toe box is often adequate treatment to relieve symptoms, allowing the condition to diminish on its own. For more severe conditions, however, additional treatment or surgery may be necessary to remove the tumor. The primary goal of most early treatment regimens is to relieve pressure on areas where a neuroma develops. Your podiatric physician will examine and likely X-ray the affected area and suggest a treatment plan that best suits your individual case. Padding and Taping. Special padding at the ball of the foot may change the abnormal foot function and relieve the symptoms caused by the neuroma. Medication. Anti-inflammatory drugs and cortisone injections can be prescribed to ease acute pain and inflammation caused by the neuroma. Orthotics. Custom shoe inserts made by your podiatrist may be useful in controlling foot function. Orthotics may reduce symptoms and prevent the worsening of the condition.

Surgical Treatment
About one person in four will not require any surgery for Morton's neuroma and their symptoms can be controlled with footwear modification and steroid/local anaesthetic injections. Of those who choose to have surgery, about three out of four will have good results with relief of their symptoms. Recurrent or persisting (chronic) symptoms can occur after surgery. Sometimes, decompression of the nerve may have been incomplete or the nerve may just remain 'irritable'. In those who have had cutting out (resection) of the nerve (neurectomy), a recurrent or 'stump' neuroma may develop in any nerve tissue that was left behind. This can sometimes be more painful than the original condition.
Prevention
Ensuring that shoes are well fitted, low-heeled and with a wide toe area may help to prevent Morton's neuroma.
How Shoe Lifts Cure Leg Length Discrepancy
There are not one but two different types of leg length discrepancies, congenital and acquired. Congenital means you are born with it. One leg is structurally shorter than the other. As a result of developmental phases of aging, the human brain senses the stride pattern and recognizes some difference. Your body usually adapts by dipping one shoulder to the "short" side. A difference of under a quarter inch is not blatantly excessive, require Shoe Lifts to compensate and usually won't have a serious effect over a lifetime.

Leg length inequality goes largely undiagnosed on a daily basis, however this condition is very easily solved, and can eliminate a number of instances of lumbar pain.
Treatment for leg length inequality usually involves Shoe Lifts. Many are very inexpensive, in most cases being less than twenty dollars, compared to a custom orthotic of $200 plus. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Lower back pain is easily the most prevalent health problem affecting men and women today. Around 80 million men and women experience back pain at some point in their life. It is a problem that costs companies millions of dollars annually on account of lost time and production. New and superior treatment solutions are continually sought after in the hope of reducing the economic influence this issue causes.

People from all corners of the world suffer from foot ache as a result of leg length discrepancy. In a lot of these cases Shoe Lifts are usually of very beneficial. The lifts are capable of easing any pain and discomfort in the feet. Shoe Lifts are recommended by countless qualified orthopaedic practitioners".
In order to support the human body in a well balanced fashion, feet have a vital part to play. Despite that, it can be the most neglected region in the human body. Some people have flat-feet meaning there may be unequal force exerted on the feet. This causes other areas of the body including knees, ankles and backs to be affected too. Shoe Lifts guarantee that ideal posture and balance are restored.

Leg length inequality goes largely undiagnosed on a daily basis, however this condition is very easily solved, and can eliminate a number of instances of lumbar pain.
Treatment for leg length inequality usually involves Shoe Lifts. Many are very inexpensive, in most cases being less than twenty dollars, compared to a custom orthotic of $200 plus. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Lower back pain is easily the most prevalent health problem affecting men and women today. Around 80 million men and women experience back pain at some point in their life. It is a problem that costs companies millions of dollars annually on account of lost time and production. New and superior treatment solutions are continually sought after in the hope of reducing the economic influence this issue causes.

People from all corners of the world suffer from foot ache as a result of leg length discrepancy. In a lot of these cases Shoe Lifts are usually of very beneficial. The lifts are capable of easing any pain and discomfort in the feet. Shoe Lifts are recommended by countless qualified orthopaedic practitioners".
In order to support the human body in a well balanced fashion, feet have a vital part to play. Despite that, it can be the most neglected region in the human body. Some people have flat-feet meaning there may be unequal force exerted on the feet. This causes other areas of the body including knees, ankles and backs to be affected too. Shoe Lifts guarantee that ideal posture and balance are restored.
How Shoe Lifts Cure Leg Length Discrepancy
There are actually two unique variations of leg length discrepancies, congenital and acquired. Congenital means you are born with it. One leg is anatomically shorter compared to the other. As a result of developmental periods of aging, the human brain picks up on the step pattern and identifies some difference. Your body typically adapts by tilting one shoulder to the "short" side. A difference of under a quarter inch is not really uncommon, demand Shoe Lifts to compensate and usually does not have a profound effect over a lifetime.

Leg length inequality goes typically undiagnosed on a daily basis, yet this problem is very easily remedied, and can eliminate quite a few cases of lower back pain.
Therapy for leg length inequality usually involves Shoe Lifts. They are low cost, regularly being below twenty dollars, in comparison to a custom orthotic of $200 if not more. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Back pain is the most widespread ailment afflicting men and women today. Around 80 million men and women suffer from back pain at some point in their life. It's a problem which costs companies huge amounts of money year after year on account of lost time and productivity. New and more effective treatment solutions are continually sought after in the hope of decreasing the economic influence this issue causes.

Men and women from all corners of the earth suffer from foot ache due to leg length discrepancy. In most of these situations Shoe Lifts are usually of very useful. The lifts are capable of decreasing any discomfort in the feet. Shoe Lifts are recommended by many certified orthopaedic practitioners".
In order to support the human body in a well balanced fashion, feet have got a significant part to play. Irrespective of that, it's often the most neglected zone in the body. Many people have flat-feet meaning there may be unequal force exerted on the feet. This will cause other body parts including knees, ankles and backs to be affected too. Shoe Lifts make sure that suitable posture and balance are restored.

Leg length inequality goes typically undiagnosed on a daily basis, yet this problem is very easily remedied, and can eliminate quite a few cases of lower back pain.
Therapy for leg length inequality usually involves Shoe Lifts. They are low cost, regularly being below twenty dollars, in comparison to a custom orthotic of $200 if not more. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Back pain is the most widespread ailment afflicting men and women today. Around 80 million men and women suffer from back pain at some point in their life. It's a problem which costs companies huge amounts of money year after year on account of lost time and productivity. New and more effective treatment solutions are continually sought after in the hope of decreasing the economic influence this issue causes.

Men and women from all corners of the earth suffer from foot ache due to leg length discrepancy. In most of these situations Shoe Lifts are usually of very useful. The lifts are capable of decreasing any discomfort in the feet. Shoe Lifts are recommended by many certified orthopaedic practitioners".
In order to support the human body in a well balanced fashion, feet have got a significant part to play. Irrespective of that, it's often the most neglected zone in the body. Many people have flat-feet meaning there may be unequal force exerted on the feet. This will cause other body parts including knees, ankles and backs to be affected too. Shoe Lifts make sure that suitable posture and balance are restored.
What Exactly Is Heel Spur

Overview
The two most common causes of pain in the bottom of the heel, the arch, or both the heel and the arch, are heel spurs and plantar fasciitis. A Heel Spur is a piece of calcium or bone that sticks out from the bottom of the heel bone, and lies within the fibers of the plantar fascia. When walking, the spur digs into the plantar fascia and causes small micro-tears in the plantar fascia. This produces inflammation and pain in the heel, which at times may radiate into the arch.
Causes
The calcaneal spur is seen most often in persons over the age of 40. The condition can also be associated with osteoarthritis, rheumatoid arthritis, poor circulation of the blood and other degenerative diseases. Men and women are equally likely to have them.

Symptoms
More often than not, heel spurs have no signs or symptoms, and you don?t feel any pain. This is because heel spurs aren?t pointy or sharp pieces of bone, contrary to common belief. Heel spurs don?t cut tissue every time movement occurs; they?re actually deposits of calcium on bone set in place by the body?s normal bone-forming mechanisms. This means they?re smooth and flat, just like all other bones. Because there?s already tissue present at the site of a heel spur, sometimes that area and the surrounding tissue get inflamed, leading to a number of symptoms, such as chronic heel pain that occurs when jogging or walking.
Diagnosis
A Heel Spur diagnosis is made when an X-ray shows a hook of bone protruding from the bottom of the foot at the point where the plantar fascia is attached to the heel bone. The plantar fascia is the thick, connective tissue that runs from the calcaneus (heel bone) to the ball of the foot. This strong and tight tissue helps maintain the arch of the foot. It is also one of the major transmitters of weight across the foot as you walk or run. In other words, tremendous stress is placed on the plantar fascia.
Non Surgical Treatment
Over-the-counter or prescription-strength anti-inflammatory medications can help temporarily, but can cause side effects with prolonged use - the most significant being gastrointestinal upset, ulceration and bleeding. Deep tissue massage, taping and other physical therapy modalities can also be helpful. Arch support is highly recommended, either with shoe inserts or custom orthotics made by podiatrists. If pain continues, a steroid injection at the site of pain may be recommended; however, many physicians do not like injecting around the heel. The side effects of steroids injected in this area can be serious and worsen symptoms. Complications can include fat necrosis (death of fatty tissue) of the heel and rupture of the plantar fascia.
Surgical Treatment
Usually, heel spurs are curable with conservative treatment. If not, heel spurs are curable with surgery, although there is the possibility of them growing back. About 10% of those who continue to see a physician for plantar fascitis have it for more than a year. If there is limited success after approximately one year of conservative treatment, patients are often advised to have surgery.
Have I Got Heel Spur
Overview
Patients and doctors often confuse the terms heel spur and plantar fasciitis. While these two diagnoses are related, they are not the same. Plantar fasciitis refers to the inflammation of the plantar fascia--the tissue that forms the arch of the foot. A heel spur is a hook of bone that can form on the heel bone (calcaneus) and is associated with plantar fasciitis. About 70 percent of patients with plantar fasciitis have a heel spur that can be seen on an X-ray. However, many patients without symptoms of pain can have a heel spur. The exact relationship between plantar fasciitis and heel spurs is not entirely understood.
Causes
The calcaneal spur is seen most often in persons over the age of 40. The condition can also be associated with osteoarthritis, rheumatoid arthritis, poor circulation of the blood and other degenerative diseases. Men and women are equally likely to have them.

Symptoms
The spur itself is not painful, however, if it is sharp and pointed it can poke into soft tissue surrounding the spur itself. As the bone spur irritates the tissue, inflammation and bruising can occur leading to heel pain. Heel spurs can affect your ability to do your usual work and/or activities, and can also trap and irritate the nerves in your heel area. They can change the way you walk, and can lead to knee, hip and low back injuries. If severe, they may require medical intervention.
Diagnosis
Heel spurs and plantar fasciitis are diagnosed based on the history of pain and tenderness localized to these areas. They are specifically identified when there is point tenderness at the bottom of the heel, which makes it difficult to walk barefoot on tile or wood floors. X-ray examination of the foot is used to identify the bony prominence (spur) of the heel bone (calcaneus).
Non Surgical Treatment
Treatments for bone spurs and plantar fasciitis include Stretching the calf muscles several times daily is critical in providing tension relief for the plantar fascia. Some physicians may recommend using a step to stretch, while others may encourage yoga or pushing against a wall to stretch. Icing after activity. A frozen tennis ball can provide specific relief. Rolling the tennis ball under the arch of the foot after exercise can lessen pain in the area. Taping is also recommended at times. Several manufacturers of sports tape have plantar fascia specific lines. Orthotics are a good idea for those on their feet during the day. Orthotics can provide cushioning and relief. Cortisone shots in the fascia can provide temporary anti-inflammatory relief. Losing weight is perhaps the most effective method of improving heel and foot pain. Those who are overweight are far more likely to report these syndromes.
Surgical Treatment
When chronic heel pain fails to respond to conservative treatment, surgical treatment may be necessary. Heel surgery can provide relief of pain and restore mobility. The type of procedure used is based on examination and usually consists of releasing the excessive tightness of the plantar fascia, called a plantar fascia release. Depending on the presence of excess bony build up, the procedure may or may not include removal of heel spurs. Similar to other surgical interventions, there are various modifications and surgical enhancements regarding surgery of the heel.
Prevention
A variety of steps can be taken to avoid heel pain and accompanying afflictions. Wear shoes that fit well-front, back, and sides-and have shock-absorbent soles, rigid shanks, and supportive heel counters. Wear the proper shoes for each activity. Do not wear shoes with excessive wear on heels or soles. Prepare properly before exercising. Warm up and do stretching exercises before and after running. Pace yourself when you participate in athletic activities. Don't underestimate your body's need for rest and good nutrition. If obese, lose weight.